The Medicare Access and CHIP Reauthorization Act (MACRA) was enacted in April 2015 and is being implemented by the Centers for Medicare and Medicaid Services (CMS). With a goal towards improving patient-centric care, MACRA makes fundamental changes to Medicare payments and quality reporting for provider services in 3 ways. These changes create a Quality Payment Program (QPP):
- End SGR - Ending the Sustainable Growth Rate (SGR) formula for determining Medicare payments for health care providers’ services.
- Reward Better Care - Making a new framework for rewarding health care providers for giving better care not just more care
- Consolidate CMS Reporting - Combining existing CMS quality reporting into one new system
Providers may take one of two paths to participate in the QPP which is either the Merit-Based Incentive Payment System (MIPS) or the Alternative Payment Model (APM).
Merit-Based Incentive Payment System (MIPS)
This is a new program that combines 3 independent programs and adds a fourth component to promote ongoing improvement and innovation. A goal of MIPS is to provide Eligible Clinicians (ECs) the flexibility to choose activities and measures that are most meaningful to their practice to demonstrate performance. ECs may report as individuals or as a group. The four components for reporting are:
- Quality: Replaces the Physician Quality Reporting System (PQRS) and reduces the required measured from 9 to 6. Year 1 weight 50%.
- Advancing Care Information: Replaces the EHR Incentive, Meaningful Use for Medicare Part B with a focus on patient electronic access, coordination of care through patient engagement, and health IT interoperability. Year 1 weight 25%
- Resource Use: Replaces the Value Modifier with an added 40+ episode specific measures to address specialty concerns. Year 1 weight 10%.
- Clinical Practice Improvement Activities: New measure that requires a minimum selection of one Clinical Practice Improvement Activity (CPIA) with full credit given for patient-centered medical home or a comparative specialty. Year 1 weight 15%.
The Composite Performance Score (CPS) for MIPS will be calculated from these four weighted components and the CPS published on the CMS Physician Compare website. As it pertains to payments, MACRA requires MIPS to be budget neutral. Therefore, the scores would be aggregated and positive and negative payment adjustments would be calculated to achieve budget neutrality. The adjustments start at +4% and increase annually until +9% is reached. The Center for Medicare and Medicaid Services (CMS) will measure performance for Eligible Clinicians starting January 1, 2017 with payments based on those measures beginning in 2019.
Alternative Payment Models (APMs)
APMs are risk-based arrangements between providers and payers such as Next Generation Accountable Care Organizations (ACOs). MACRA will only consider Advanced APMs as those eligible for this QPP path. These arrangements have the following basic characteristics:
- Risk - Require participants to bear a certain amount of financial risk.
- Quality Measures - Base payments on quality measures comparable to those used in the MIPS quality performance category.
- EHR - Require participants to use certified EHR technology.
According to the Healthcare Financial Management Association (HMFA), the MACRA rule identified these specific eligible APMs will qualify for bonus payments and an exemption from MIPS reporting.
- Next Generation ACO
- Comprehensive Primary Care Plus (CPC+)
- Medicare Shared Savings Program (MSSP) Tracks 2 and 3
- Oncology Care Model with two-sided risk
- Comprehensive ESRD Care (for large dialysis organizations)
Although only a small number of providers are Qualifying APM Participant (QP) in Advanced APMs, CMS believes this will be the preferred choice over the long-term.
Timeline
The final rule was recently released by CMS on October 14, 2016. The timeline is aggressive with the first performance year starting on January 1, 2017 and payments in 2019. The current CMS timeline illustrates the transition to MIPS and certain APMs.
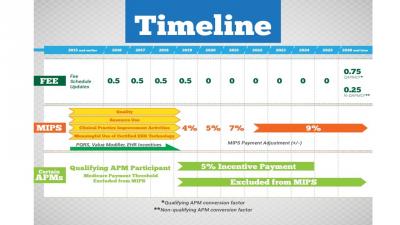
Source: CMS Timeline
In preparation for January 1, 2017, Acting Administrator Andy Slavitt has outlined four different options to allow physicians to pick their pace of participation for 2017.
Option 1: Test the Quality Payment Program: Providers will avoid a negative payment adjustment as long as some data is submitted to the QPP in 2017. This option is designed to allow testing and preparation for a broader participation in 2018 and beyond.
Option 2: Participate for part of the calendar year: Providers may qualify for a small payment if data is submitted to the QPP for a part of the calendar year in 2017.
Option 3: Participate for the full calendar year: Providers may qualify for a modest payment adjustment if data is submitted to the QPP for the entire calendar year in 2017.
Option 4: Participate in an Advanced APM in 2017: Providers would qualify for a 5% incentive payment in 2019 if the provider is a qualified participant in an Advanced APM and a certain threshold of Medicare payments or patients are met.
Summary
The current Medicare population is estimated at over 56 million lives and growing which makes the status quo of rising healthcare costs unsustainable. MACRA presents a significant shift from fee-for-service to value-based reimbursement with many proponents and critics. There is considerable anxiety within the physician community with one of the biggest concerns being that the quality initiatives will favor larger practices who are in a stronger position to meet the reporting requirements. In an attempt to ease fears, CMS has allocated $100M over the next 5 years to help small practices get up to speed. Like it or not, it seems that value-based payments are here to stay.
This Insight is intended to be a general summary as of the published date. As CMS policy frequently changes and evolves, Ninestone Corporation keeps itself apprised of updates and can help evaluate how policies and trends impact your business. Contact us today to discuss your healthcare business needs.
Tammy Chu, Ninestone Senior Consultant
October, 2016
